Learn more about
Regain Control with Evidence-Based Pelvic Health Physical Therapy
Urinary and fecal incontinence are common yet under-addressed pelvic floor disorders that affect individuals across all stages of life. These conditions involve the involuntary loss of urine or stool and may result from pelvic floor dysfunction, neurological conditions, childbirth, aging, surgery, or other medical factors.
While these symptoms are prevalent, they are not a normal part of aging and should not be dismissed as inevitable. Left untreated, incontinence can significantly impact quality of life, emotional well-being, and daily function.
At Pelvic Health Solutions, our team of specialized physical therapists treats the full spectrum of incontinence, including:
Leakage that occurs during physical activity, such as coughing, sneezing, or exercise.
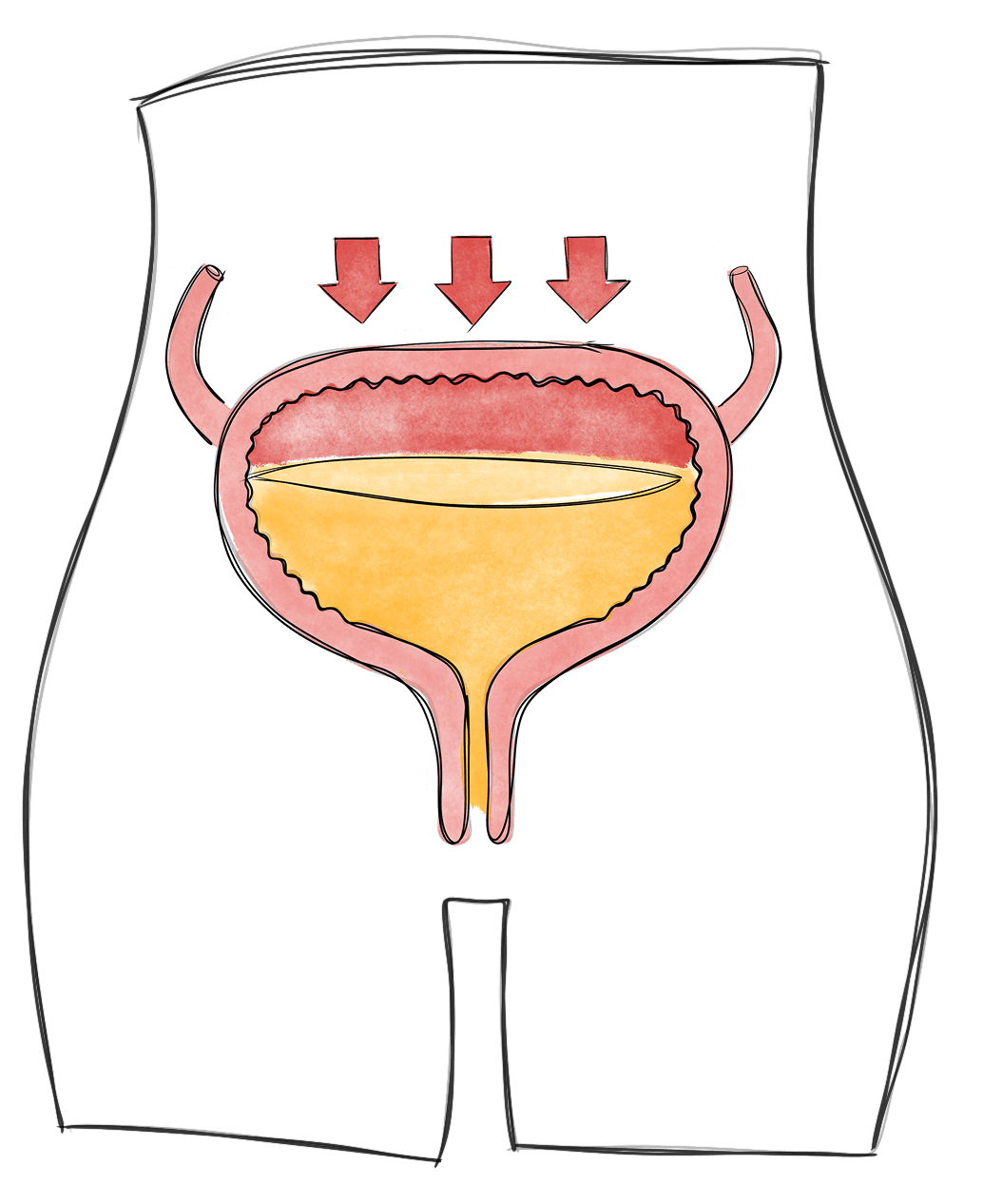
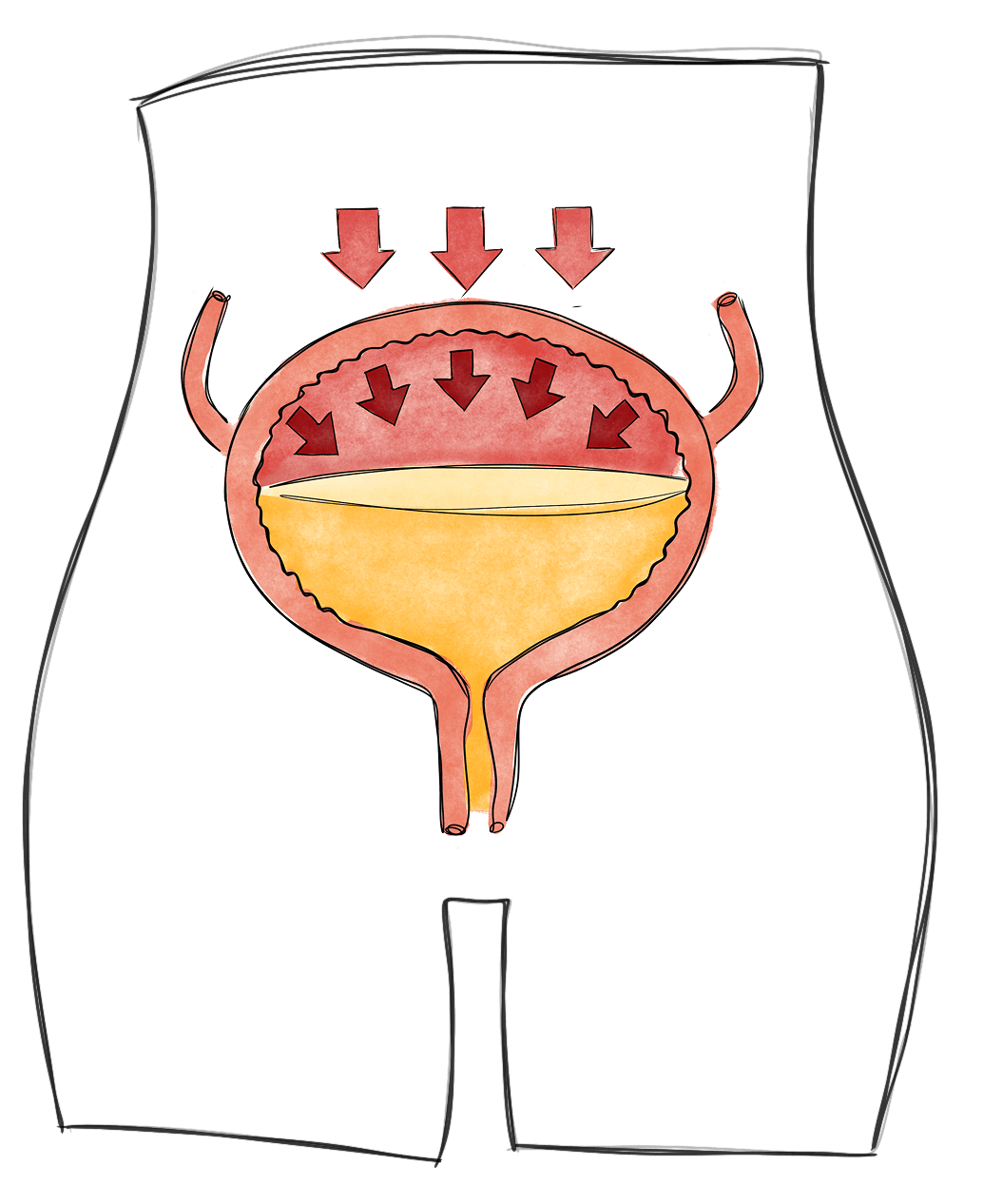
Stress incontinence occurs when pressure on the bladder—such as during coughing, laughing, sneezing, or exercise—causes urine to leak. It's often related to weakened or underactive pelvic floor muscles and insufficient support around the urethra.
A sudden, intense urge to urinate followed by involuntary loss of urine.
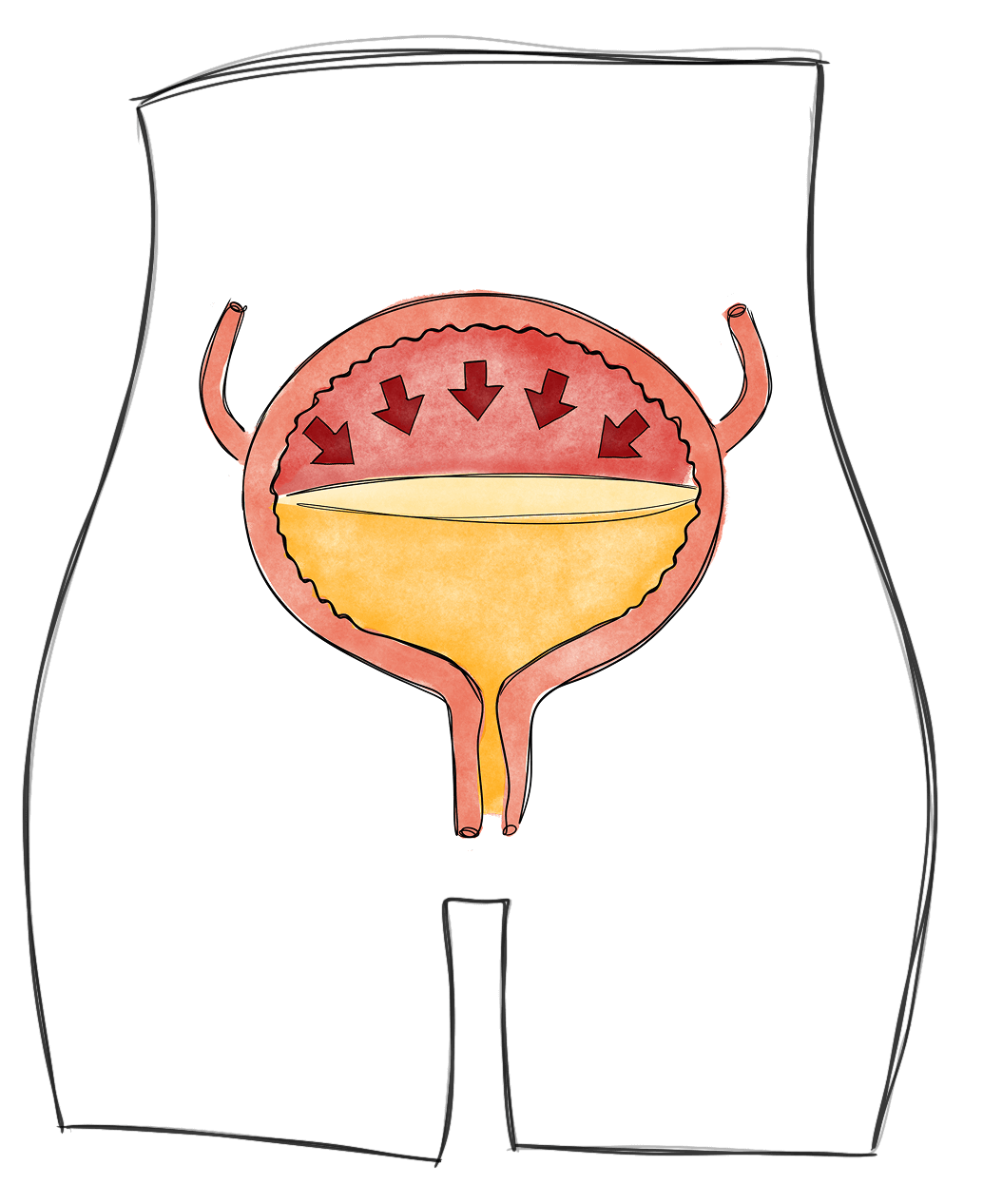
Also known as overactive bladder, urge incontinence involves a sudden, strong need to urinate followed by leakage. It may be caused by bladder muscle overactivity, irritation, or disrupted nerve signals between the bladder and brain.
Incontinence is a medical condition that can and should be addressed. Delaying treatment may lead to increased severity, higher risk of falls (particularly in older adults), skin irritation or infection, and decreased physical activity or social participation.
More importantly, effective treatment is available—and supported by strong clinical evidence.
Pelvic health physical therapy is a first-line, non-surgical treatment for urinary and fecal incontinence. At Pelvic Health Solutions, we provide individualized, one-on-one care rooted in current clinical guidelines and best practices.
All sessions are for a full hour in a private room and our treatment approach includes:
Our therapists undergo advanced training in pelvic health and follow evidence-based protocols tailored to your specific symptoms and goals.
We are Florida’s leading private practice pelvic health physical therapy clinic, with locations in Palm Beach Gardens, Boca Raton, Stuart and Pembroke Pines. Our team is known for compassionate, trauma-informed care that integrates clinical expertise with whole-person healing.
We treat all genders and life stages, including those experiencing intimacy-related pain due to postpartum changes, menopause, pelvic surgery, trauma, or chronic pelvic pain.
It was absolutely worth going.
I had done pelvic floor therapy before—about nine years ago, after my second child. I was diagnosed with a rectocele. I didn’t even know what that was at the time, but I had really big babies and a lot of trauma down there. I had no muscle control. The exercises were intense and time-consuming, but I was very dedicated, and after nine sessions, I was good to go…
“I was very skeptical of my first visit, thinking ‘How could physical therapy help my stress incontinence? This must be a scam.’ How wrong I was! My therapist was extremely professional and explained every procedure and exercise in detail so that I was comfortable – and more importantly, so I understood the mechanics of all of the muscles and the resulting issues. I have seen a remarkable improvement and can now enjoy simple things like taking a walk and laughing without embarrassment. It feels good to exercise again, too! Words can’t express my appreciation for helping to get my life back to normal! My only regret is that I didn’t find you sooner!”
“As a physician who practiced for more than 40 years, I often had female patients with urinary incontinence and male patients post prostatectomy. It wasn’t until I underwent the prostatectomy myself that I understood the importance of pelvic floor therapists and the importance of doing the exercises correctly. I was able to regain continence after only 6 weeks post op and the exercises were helpful from a sexual standpoint as well. I would recommend men who are undergoing prostatectomy to begin seeing you one month before the procedure to start therapy. If any of your male patients would like to talk to me about my experience I would be glad to help. Thank you again for your superb care.”
“I had a robotic surgical radical prostatectomy. I was operated on November 2017 and I had the usual and anticipated incontinence and erectile dysfunction (ED). I was prepared by the surgeon and his staff to expect this during the first year. Post operatively Gail worked with me and made me realize the variety of ways the pelvic floor muscles move and constrict in order to control bodily functions we of course all take for granted. The anatomy is really complicated and once you understand this it really helps with your recovery. I followed her instructions over the next several months postoperatively and my incontinence as a result was short lived. The incontinence is almost always correctable with well-done pelvic floor therapy. — Dr. B. FL
“Thank you very much for guiding me through my pelvic floor strengthening after my prostatectomy with Dr. Vipul Patel, a world-renowned surgeon in Celebration, FL. After undergoing a very successful surgery, his office referred me to you for follow up therapy to facilitate my return to urinary continence. The seven therapy sessions I received from you were extremely beneficial in strengthening my pelvic floor and returning me to a normal post-surgery life. I would strongly recommend that any man experiencing prostate cancer should select follow-up pelvic floor therapy with you. — S.H.
I have a severe bladder incontinence. In a review, I had a choice of two options, a cathetor or surgery. I found Pelvic Health Solutions in Palm Beach Gardens, Florida. I work with Tiffany Grigsby D.P.T. Doctor of P.T. For the bladder. She is patient, very knowledgeable, explains & reviews my progress. A blessing. I am so improved. The facility is not large. Compact. The office is managed by Kim Sherral and Jennifer. You are given printed appointments, reminder calls, and follow ups. They work to accommodate you.
Many patients come to us after feeling rushed, overlooked, or given a one-size-fits-all plan elsewhere. Exceptional pelvic health care requires time, expertise, and individualized attention—conditions that traditional insurance models simply don’t allow.
Our out-of-network structure is intentional. It allows us to deliver the level of care you deserve.
Patients often find that investing in specialized, expert-led care leads to faster, more meaningful improvement—and ultimately reduces the time, cost, and frustration spent on ineffective or fragmented treatments.
At Pelvic Health Solutions, you receive care designed around you: private, precise, and rooted in clinical excellence.
Pelvic health physical therapy is a specialized area of physical therapy that focuses on assessing and treating conditions related to the pelvic floor muscles, ligaments, and connective tissues. The pelvic floor plays a crucial role in supporting the pelvic organs, controlling bladder and bowel function, and contributing to sexual health.
Pelvic health physical therapy focuses on the muscles, tissues, and organs specifically in the pelvic area, which include the bladder and bowel. It helps with problems like pelvic pain, urinary or bowel issues, and discomfort during sex.
Orthopedic physical therapy, on the other hand, deals with muscles and joints in other parts of the body, like the arms, legs, and back, to help with pain, stiffness, and injuries in those areas.
pulvinar dapibus leo.
elvic floor physical therapy applies to individuals with a range of symptoms. Some of the most common ones we see are:
Pelvic Pain: Chronic pelvic pain, pain during intercourse (dyspareunia), tailbone pain, or pain in the pelvic region with movement, sitting, or pressure.
Urinary Symptoms: Urinary incontinence (leakage of urine), urinary urgency or frequency, difficulty emptying the bladder, or nocturia (excessive nighttime urination).
Bowel Symptoms: Fecal incontinence (involuntary leakage of stool or gas), constipation, rectal pain/spasms, or difficulty with bowel movements.
Pregnancy and Postpartum: Pelvic health physical therapy can help prepare the pelvic floor for childbirth and address postpartum issues such as pelvic organ prolapse, perineal pain, or diastasis recti.
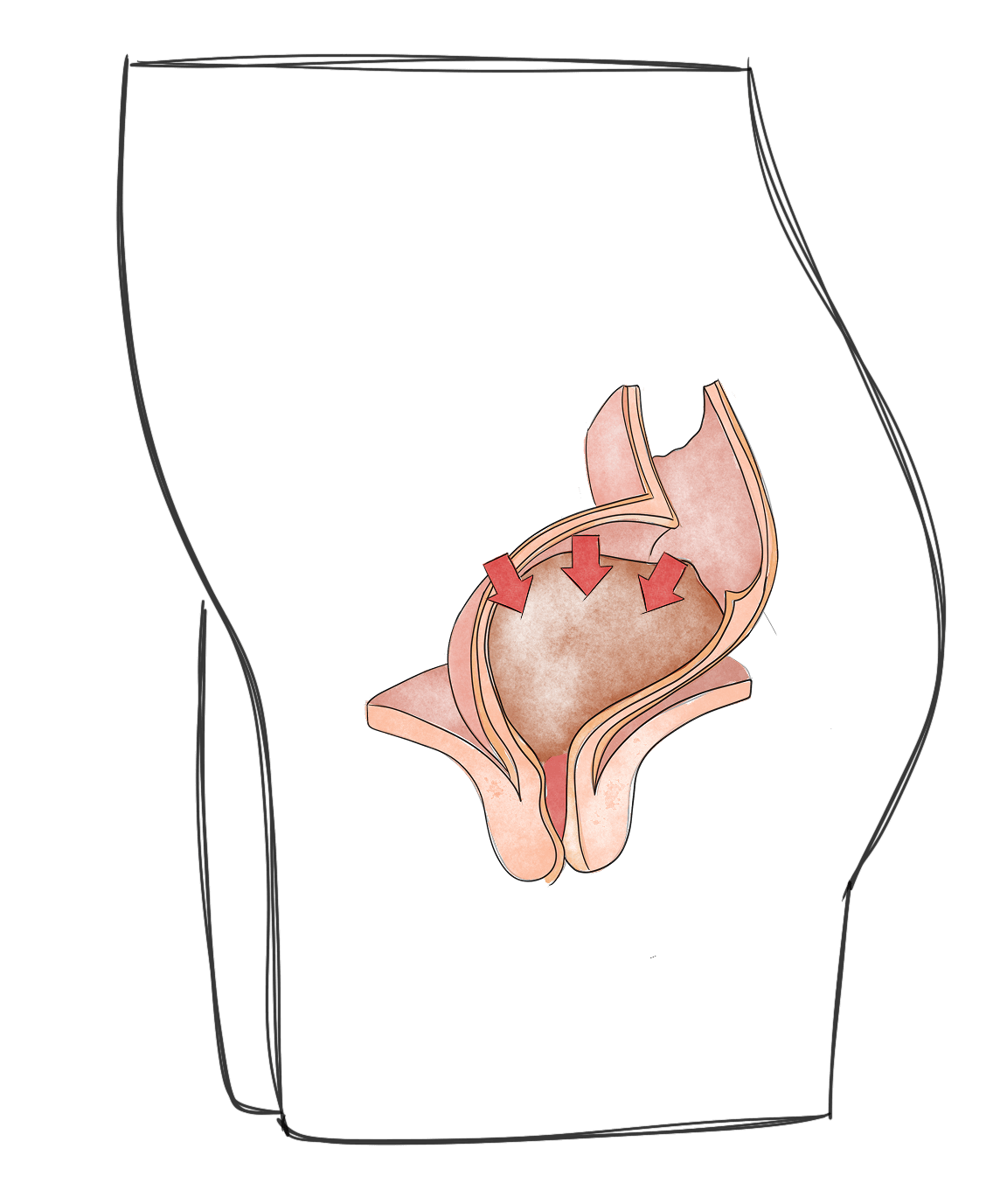
Pelvic Organ Prolapse: Descending or bulging of pelvic organs (such as the bladder, uterus, or rectum) into the vaginal canal.
Male Pelvic Conditions: Chronic pelvic pain in men, chronic prostatitis, and post-prostatectomy
If you’re considering scheduling your first visit, here’s what you can expect during the initial evaluation:
A comprehensive and respectful conversation
We begin by listening. All appointments are one-on-one with a dedicated pelvic floor physical therapist, in a private treatment room, for a full hour.
In your first session, your therapist will conduct a detailed medical and lifestyle history to better understand your symptoms, goals, and day-to-day function. Topics may include bladder, bowel, and sexual health—always discussed with care, professionalism, and respect for your comfort.
Clinical education tailored to you
You’ll receive clear, expert guidance on how the pelvic floor works, what may be contributing to your symptoms, and how physical therapy can help. Research shows that patients who understand their conditions have better outcomes. We prioritize education, and not just exercises, in your care so that you understand the why and how of your symptoms.
A thorough assessment
We assess posture, movement patterns, core stability, hip strength, breathing, and pelvic alignment. With your consent, we may offer an external and internal pelvic floor exam to assess strength, tone, and coordination. This is always optional and based on your comfort.
A personalized treatment plan
Before the session ends, your therapist will walk you through their findings and recommend a tailored and individualized plan for therapy — outlining what care may look like in the weeks ahead.
Our care model is centered around one-on-one treatment, clinical excellence, and compassionate support. We’re referred by over 100 doctors and have helped more than 5000 patients restore function, reduce symptoms, and feel confident in their bodies again.
Don’t struggle with your symptoms alone. Reach out to speak with one of our pelvic floor physical therapists.
Just like other therapies, it takes time and consistency to notice improvement. Healing time varies for each person. Some people might start feeling better after a few sessions, while others might need more time. It depends on how severe your symptoms are and how well you stick to your treatment plan.
Typically, we see our patients 1-2 times per week in order to make the most optimal recovery. Your therapist will work with you to create a plan that fits your needs and that helps you feel better as soon as possible!