The difference between common pelvic pain diagnoses and how they impact treatment.
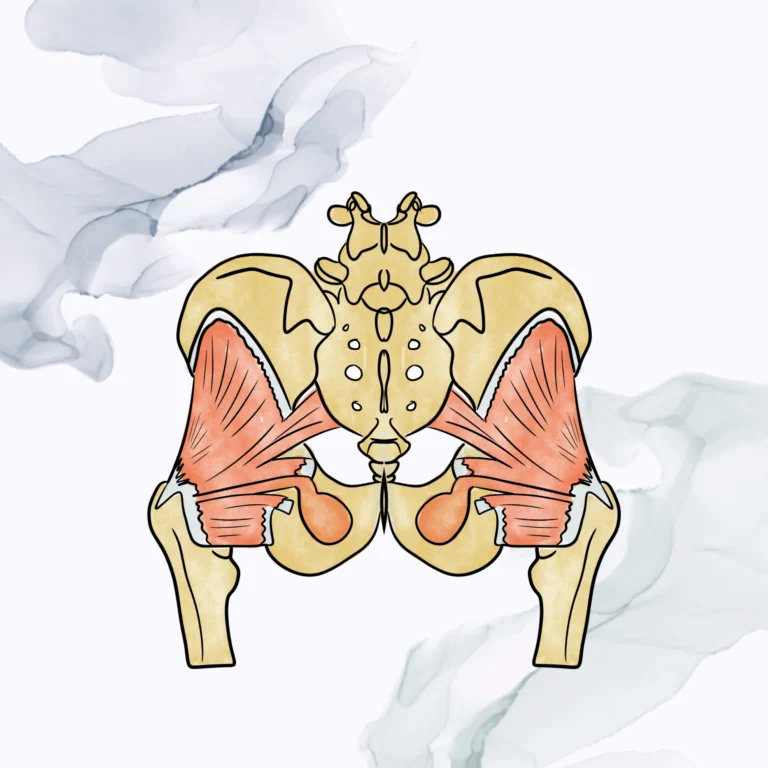
Pelvic pain is often defined as any pain confined to the general torso area from your ribcage down to your genital area. Pelvic pain can stem from several origins: digestive organs, bladder, reproductive organs and structures, and bowels/rectum. Pelvic pain is an unspecific term that includes a variety of dysfunctions and diseases. Below, we will exam some common pelvic pain diagnosis. This list does not encompass all pelvic pain-related issues, and you should speak to your current health care provider if you believe pelvic floor PT can help you!
Dyspareunia: Dyspareunia is a very general term to describe any pelvic pain during sexual intercourse. This pain can be upon initial penetration or deeper penetration. This pain can be short-lived discomfort or a long-lasting pelvic ache. Dyspareunia can contribute to decreased intimacy between sexual partners, feelings of dissatisfaction, and a negative outlook toward sex. Dyspareunia can be caused by a variety of factors such as improper lubrication, poor positioning during intercourse, muscle spasms, poor tissue health, underlying conditions or hormone imbalance. Treatment for dyspareunia includes pelvic floor down training or relaxation, diaphragmatic breathing, potential dilator training or wand training, education on different positions during sexual intercourse, and promoting surrounding muscle and soft tissue extensibility. Dyspareunia is unique to the person experiencing it and should be treated as such. Pelvic floor PT’s are specially trained in determining the best treatment path for you.
Vaginismus: Vaginismus is a more specific dysfunction which describes pelvic muscle spasm in response to penetration of the vaginal canal. Vaginismus is most often a concern when one determines they cannot insert a tampon, participate in a gynecological examination, or participate in sexual intercourse or vaginal penetration in any form. Vaginismus involves pelvic floor muscle spasm that can be accompanied by extreme pain and anxiety. Different than vaginal stenosis (true narrowing of the vaginal canal), vaginismus is a reflexive narrowing of the vaginal canal due to muscle guarding.
As the saying goes, “you never touch a hot stove twice.” Touching a hot stove causes your arm to reflexively pull back and away from the heat source. The same thing is happening with your pelvic floor muscles as a response to pain. Once you experience pain in the pelvic floor/vaginal/vulvar region, your muscles will tense up to guard in future, potentially pain-provoking events. It is on a feedback loop that consistently sends this message out in response to vaginal penetration. It is possible to “rewire” this feedback loop and prevent the spasms. This requires graded desensitization techniques, dilator training, and promoting positive feelings towards sex and vaginal penetration. Pelvic floor PT can help retrain your pelvic floor muscles and promote improved ability to insert a tampon and participate in gynecological exams and sexual intercourse.
Vestibulodynia/Vulvodynia: This terminology is interchangeable. Vulvodynia is described as discomfort, pain, and itching in the vestibule (opening to the vagina), inner labia, or vulvar tissue. This pain is generally provoked through contact with this area via touch, clothing, or the surface you sit on. This pain is usually described as “raw” or “burning” pain. Vulvodynia can be treated through graded exposure and desensitization techniques, proper vulvar-vaginal hygiene habits, promoting tissue health, and education on good seat surface options for you.
Endometriosis: Endometriosis occurs when there is regurgitation of menstrual blood out of the fallopian tubes into the body. This blood specifically contains endometrial tissue which can lead to scar tissue build up throughout the body. Scar tissue build up is generally seen within the abdomen region – but can travel up towards the eyes and brain. Our body likes to move freely (including our organs), but scar tissue can bind down reproductive organs, bladder, bowels, and digestive organs making mobility difficult. Though we cannot stop the damage done by endometriosis, we can address the mobility dysfunctions that occur with it. We provide treatment for myofascial restrictions, soft tissue mobilization, scar tissue breakdown, and visceral mobilization. These hands-on treatments provide the body movement it needs to improve mobility between your organs/intestines and promote scar tissue breakdown within the body.
Vaginal Stenosis: Vaginal stenosis is the narrowing of the vaginal canal. It can occur rarely via birth (primary stenosis), or it can happen because of external factors (disease, infection, radiation, etc.) which is considered secondary stenosis. Vaginal stenosis can cause pain with sexual intercourse, muscle spasms, and overall vaginal discomfort. Treatment may include dilator therapy which works to expand the vaginal canal and promote tolerance to penetration of the vaginal canal. Other treatments can include muscle relaxation techniques, scar tissue massage, and pelvic floor range of motion training.
Constipation: Although not solely “pelvic pain,” constipation can result in abdominal cramping. Constipation (in an otherwise healthy colon) occurs due to decreased colon motility which causes overabsorption of water in the large intestine. With decreased movement and water, stool hardens which makes it more difficult to pass. Constipation can also be caused by pelvic floor muscle spasms. As the stool passes, an overactive pelvic floor can spasm and cut off the bowel movement before it completely evacuates. This “trapped” stool then gets harder to pass as the rectum absorbs more water from it. This is known as outlet constipation. Treatments for constipation include bowel massage, addressing soft tissue restrictions, decreasing pelvic floor muscle spasms, addressing underlying diet causes, and promoting healthy water intake.
Tailbone pain: Many people have – or know of someone who has – broken their tailbone. However, the tailbone does not have to experience trauma to cause discomfort. Persistent tailbone pain (a.k.a coccydynia) is also quite common in our population. The muscles around the tailbone (pelvic floor muscles) can experience spasms which lead to tailbone discomfort or pain. Overactivity of the pelvic floor muscles on the right side can “pull” the tailbone towards the right side of the body causing asymmetry. The same thing can happen on the left. Pelvic floor physical therapy works to reduce spasm in these muscles and decrease pain associated with coccydynia.
Interstitial Cystitis: Interstitial cystitis is also known as painful bladder syndrome. Here is a link (insert link to IC article) to our article which goes more in-depth on what IC is, and how pelvic floor PT can help.
Prostatitis: Prostatitis, or pain/inflammation of the prostate, can come in many forms. Prostatitis can occur due to a bacterial infection or overactivity of the pelvic floor muscles. Prostatitis can be acute (one time occurrence lasting under 4 weeks) or chronic (recurrent bouts lasting 3 months or longer). Prostatitis can manifest in many ways such as pain in the pelvis, urinary frequency, urinary urgency, burning during urination, pain with ejaculation, or a weak urinary stream. Pelvic floor physical therapy can reduce pain and associated symptoms of prostatitis by promoting pelvic floor relaxation, biofeedback to reduce pelvic floor tone, and education on voiding techniques to reduce future occurrences of prostatitis.
This is not an exhaustive list for causes of pelvic pain, and each patient has a unique set of signs and symptoms which will guide their treatment. Unfortunately, pelvic pain diagnoses tend to overlap and contribute to increasing pain and dysfunction. Fortunately, there are solutions that can end this cycle of pain, discomfort, and frustration. Pelvic floor physical therapy can address all the above dysfunctions by treating the pelvic floor muscles, behavioral modifications, and establishing a better connection between the nervous system and pelvis.