A feeling of pressure, heaviness, or bulging in the pelvic area can be alarming. But for many people—especially after childbirth or with age—these symptoms may be a sign of pelvic organ prolapse (POP), a condition that affects nearly half of all women over the age of 50.
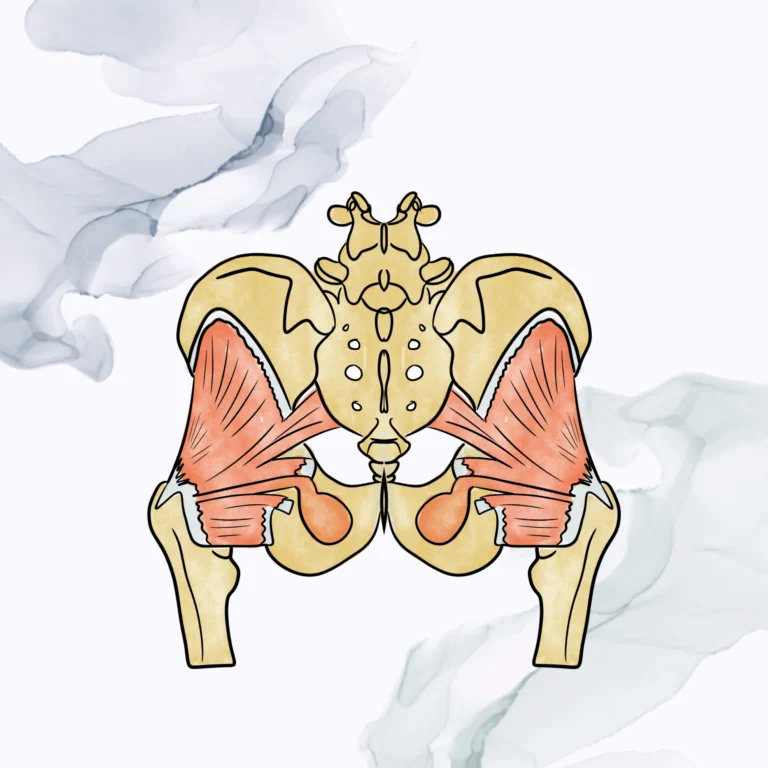
Pelvic health physical therapy is often a first-line, non-surgical approach to managing prolapse symptoms, restoring pelvic support, and improving function. If you’re experiencing pelvic pressure or discomfort, understanding how your pelvic anatomy works—and what happens when its support systems are strained—is a key step toward relief.
What Is Pelvic Organ Prolapse?
Pelvic organ prolapse occurs when the muscles, ligaments, and connective tissues of the pelvic floor become weakened or overstretched. As a result, one or more pelvic organs—such as the bladder, uterus, or rectum—can shift downward and press against the vaginal or rectal walls.
Types of prolapse include:
- Cystocele (Bladder Prolapse): The bladder bulges into the front vaginal wall.
- Rectocele (Rectal Prolapse): The rectum pushes into the back wall of the vagina.
- Uterine Prolapse: The uterus descends into the vaginal canal.
- Vaginal Vault Prolapse: The top of the vaginal wall collapses, often after hysterectomy.
- Enterocele: The small intestine descends and presses into the upper vaginal wall.
These changes often occur gradually and may vary throughout the day or with activity.
Common Symptoms of Pelvic Organ Prolapse
Not everyone with prolapse has noticeable symptoms, but for many, the effects can impact daily comfort and function. Symptoms often include:
- A sensation of pelvic heaviness, pressure, or dragging
- A visible or palpable bulge at the vaginal opening
- Difficulty emptying the bladder or bowels
- Urinary urgency or incontinence
- Constipation or incomplete evacuation
- Discomfort or pain during intercourse
Symptoms that worsen after prolonged standing, lifting, or at the end of the day
These symptoms may fluctuate depending on hormone levels, physical activity, or pelvic muscle function.
Causes and Risk Factors
Prolapse typically develops due to a combination of pressure on the pelvic organs and weakening of the structures meant to support them. Contributing factors may include:
- Vaginal childbirth, especially with prolonged pushing or assisted delivery
- Pregnancy and multiple births
- Chronic constipation or straining
- Heavy lifting or high-impact exercise
- Menopause and hormonal changes
- Pelvic surgery, such as hysterectomy
- Genetic connective tissue disorders
- Obesity or increased abdominal pressure
Symptoms can appear shortly after childbirth or emerge years later, especially if pelvic floor rehabilitation was never completed.
How Pelvic Health Physical Therapy Helps
Pelvic floor physical therapy focuses on restoring strength, coordination, and support to the muscles and tissues that hold your pelvic organs in place. It is often recommended as a first step before considering surgical options and can also support pre- and post-operative recovery.
At Pelvic Health Solutions, board-certified physical therapists conduct a comprehensive evaluation of your pelvic muscle function, breathing patterns, posture, and daily habits.
Treatment plans may include:
- Pelvic floor muscle training: Exercises that target strength, endurance, and lifting capacity
- Breath and pressure coordination: Learning how to engage the diaphragm and core to minimize downward strain
- Manual therapy: Hands-on techniques to address tightness, scar tissue, or mobility limitations
- Postural and body mechanics training: Strategies to reduce pressure during lifting, standing, or daily movement
- Bladder and bowel education: Guidance for optimal toileting and elimination habits
- Support for pessary use: If referred by your provider, we help you adjust to and use a pessary correctly
Improvement comes from more than muscle strength alone—it’s about restoring balance and control in the entire pressure management system.
When Is Surgery Considered?
Surgical repair may be recommended for advanced prolapse or when symptoms significantly impact quality of life. Even in these cases, pelvic health therapy is often part of the care plan to optimize outcomes and reduce the risk of recurrence.
Therapy may be recommended:
- Before surgery to strengthen support structures
- After surgery to restore function and address compensatory patterns
- As an ongoing tool for pressure management and long-term maintenance
You Don’t Have to Live with POP
Pelvic organ prolapse is common, but it’s not something you have to silently endure. With expert support, many people see improvement in symptoms, comfort, and quality of life.
If you’re noticing pelvic pressure, bulging, or changes in bladder or bowel function, consider a pelvic floor evaluation.
Call 561-288-2990 or fill out our contact form to schedule a one-on-one session with a board-certified pelvic health physical therapist.
We can help you feel more supported—and confident—in your body again.