Interstitial cystitis (IC) is a chronic pain condition that affects more than 12 million Americans. It is typically 2-3 times more common in women than in men and research has shown the risk of IC increased with age. IC is characterized by both pelvic pain and urinary symptoms. Patients will experience sensations of pain and pressure in the bladder area as well as lower urinary tract symptoms. It is typically diagnosed by unexplained pain and ruling out other health conditions that may cause similar symptoms. 85% of people with IC also have pelvic floor dysfunction.
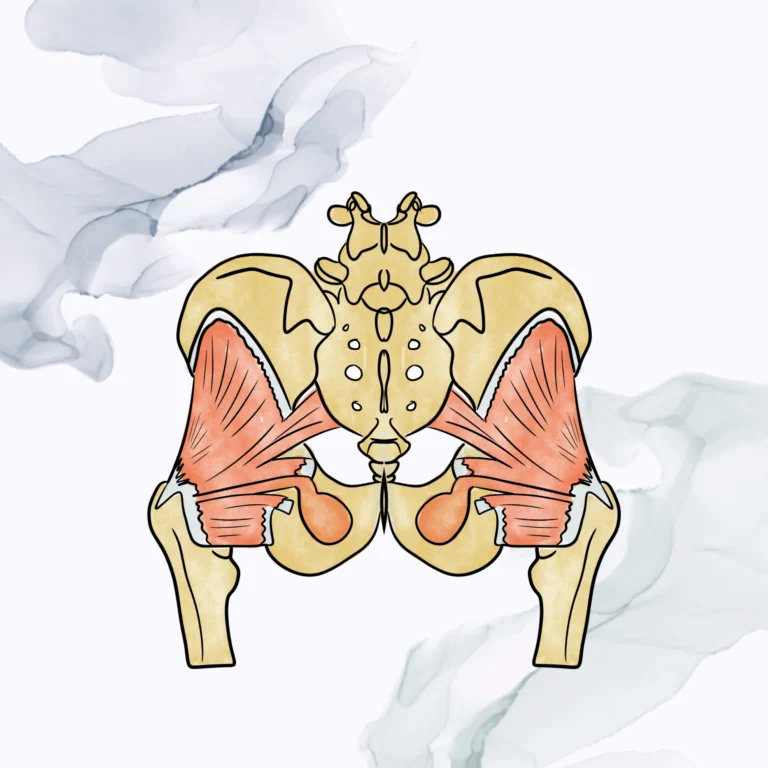
Pain is often the most common sign along with pressure of the bladder. The bladder pain may increase as the bladder fills. Pain may also be experienced in other areas of the pelvic region and low back. The muscles of the pelvic floor attach to the front (pubic bone), back (tailbone), and sides of the pelvis and help to support all of the pelvic organs as well as coordinate between contraction and relaxation to allow for proper bladder and bowel function. Often times with IC, these muscles are tight or in spasm which causes trigger points to develop. Inflammation will arise and persist due to the chronic nature of IC. Muscle tightness, trigger points, and inflammation can irritate the nerves that run through the pelvis and refer pain to other areas such as pelvis, thighs, buttocks, lower abdomen, and perineal area.
Frequency of urination is also a common symptom with IC. Typical daily voiding ranges between 5-7 times a day with no night time voiding. A patient with IC will go the bathroom to urinate more often during the day as well as at night. This can also lead to urinary urgency. Some patients will feel the urge to urinate that does not even go away after they have voided. Other symptoms that may occur with IC include burning with urination, pain with intercourse, difficulty starting/maintaining urine stream, and constipation. Symptoms may be exacerbated by various reasons. Certain foods or drinks, such as spicy foods or caffeine, may be more irritating to the bladder. Stress both physical and mental can be an irritating factor. Some women may notice symptoms vary around their period as well.
Only a fraction of patients with the key symptoms of IC (urinary frequency, urgency, and pelvic pain) have ulcers within the bladder (Hunner lesions) and many are found to not have any sort of bladder pathology at all. Thus the muscles of the pelvic floor as well as external hip/pelvic musculature are important to assess as they may aide with decreasing and managing symptoms related to IC. The American Urological Association has given pelvic floor physical therapy a grade “A” and is recommended as the first line of medical treatment for IC. Other bladder treatments and oral medication are often needed to be continued indefinitely to provide benefits if they work. Physical therapy can provide lifestyle changes and techniques for sustained relief. One study in 2013 showed that 63% of patients had significant pain improvement with pelvic floor physical therapy.
As always, a thorough initial evaluation would be completed prior to beginning treatment as everyone is individual. This would include both an external assessment of the hip/pelvic/back muscles and an internal assessment of the pelvic floor muscles. The goal of physical therapy is to restore normal function of the muscles, prevent irritation of the nerves that cause pain, and clearing inflammation from the system. Release of trigger points in the tightened muscles helps to clear inflammation in the fascia which can restore better blood flow and reduce reoccurrence of trigger points. This can help with disrupting the nervous system’s pain feedback loop. Other treatments include relaxation of the pelvic floor and hip muscles and education for self-care at home such as deep breathing, stretching and self-release of pelvic floor muscles.
Our skilled therapists at Pelvic Health Solutions can evaluate and provide individualized treatment plans for patients with IC. For more information on chronic pelvic pain or other pelvic dysfunctions, call us at (561)899-7747.
Bedaiwy MA, Patterson B, Mahajan S. Prevalence of myofascial chronic pelvic pain and the effectiveness of pelvic floor physical therapy. J Reprod Med 2013; 58: 504–510.