Types of Incontinence (Leakage)
Incontinence is leakage. Leakage can be of the bowel (stool/gas) or bladder (urine). There are several different types of incontinence, but let’s list off and define some of the more common ones. We will discuss leakage in the context of bladder and bowel.
Urgency Incontinence
Urgency related incontinence can be defined by a sense of urgency to make it to the bathroom and inability to make it to the bathroom in time. This can look like you doing the ìpotty-danceî on the way to the bathroom. Usually, people who experience urgency incontinence struggle with leakage on their way to the toilet or while undressing.
Urgency urinary incontinence would be involuntary leakage of urine (pee) before sitting on the toilet. This can happen as a result of overactive (too-tight) pelvic floor muscles, poor urgency signaling to the brain, and behavioral triggers. Behavioral triggers would be things we do on a daily basis like hearing the sound of running water, putting the key in the door, garage door rising, etc.
Urgency bowel incontinence would be involuntary leakage of stool (poop) before sitting on the toilet. This usually happens because of poor stool consistency or looser stools. It can also happen for the same reasons as urgency urinary incontinence: overactive (too-tight) pelvic floor muscles, poor urgency signaling to the brain, and behavioral triggers (stress, anxiety, running).
Stress (Exertional) Incontinence
Stress related incontinence can be defined also as exertional incontinence. This would be due to a physical stress/exertional task that causes incontinence. Common forms would be sneezing, coughing, jumping, running, laughing, lifting, etc.
This can occur with urine (pee) or stool (poop) due to increased pressure in the abdomen. Causes of stress incontinence include pelvic muscle dysfunction meaning the muscles can be too tight or not provide enough support. Tight muscles do not equal strong muscles. Usually in cases of stress incontinence, a goal of treatment involves restoring coordination to the muscle. Like patting your head and rubbing your belly, training the pelvic muscles to engage during certain movements can be the key to incontinence.
Mixed Incontinence
Mixed incontinence is a combination of stress incontinence and urgency related incontinence. Most people who have incontinence fit into this category since it is heavily a muscle issue. We typically treat this type of incontinence by addressing the urgency related incontinence and then the stress (exertional) incontinence.
Urine Specific Incontinence
Overflow Urinary Incontinence
Overflow incontinence occurs more often in men occasionally due to enlarged prostate. It is characterized by a constant leak or dribble of the bladder. Nurses, teachers, and other service industry professionals have a tendency to hold their bladder for 5+ hours. The bladder is like a balloon and it will continue to stretch depending on the demands placed on it. If you hold your bladder for longer than 5 hours regularly, you may be teaching your bladder to dampen signals. This can also cause overflow incontinence.
Functional Incontinence
Functional incontinence can occur in those who are incapable of making it onto the toilet in time due to functional capacity. This could be someone who struggles with cognitive function (dementia, stroke, etc.), poor physical ability to transfer, or other factors that limit one’s independence of making it to the toilet on time. Usually, these patients will leak before they are allowed access to the toilet via help with an aide or caregiver.
Post Void Dribble
Post void dribble is incontinence immediately upon standing up from the toilet. This usually is a result of not fully emptying your bladder. This can be mitigated with double voiding techniques such as rocking back and forth on the toilet to fully empty the bladder, using a squatty potty while emptying, and releasing overactive or tight pelvic floor muscles.
Bowel Specific Incontinence
Fecal Smearing
Fecal smearing usually occurs after a bowel movement. It is when stool is unknowingly excreted from the anus without any awareness or a slight burning sensation. Looser stool is slightly more acidic than firm stool, and this can cause some burning around the anal opening. It can happen as a result of looser stools, hemorrhoids, or nerve damage around the anal opening.
Flatulence (Gas) Incontinence
If you were in a crowded elevator and felt the need to stop the passage of gas, would you be confident in your ability to do so? Gas incontinence can happen as a result of pelvic muscle dysfunction and can cause significant embarrassment and decreased quality of life. Controlling passing gas can be a critical part of pelvic floor health that can often be overlooked.
In Summary
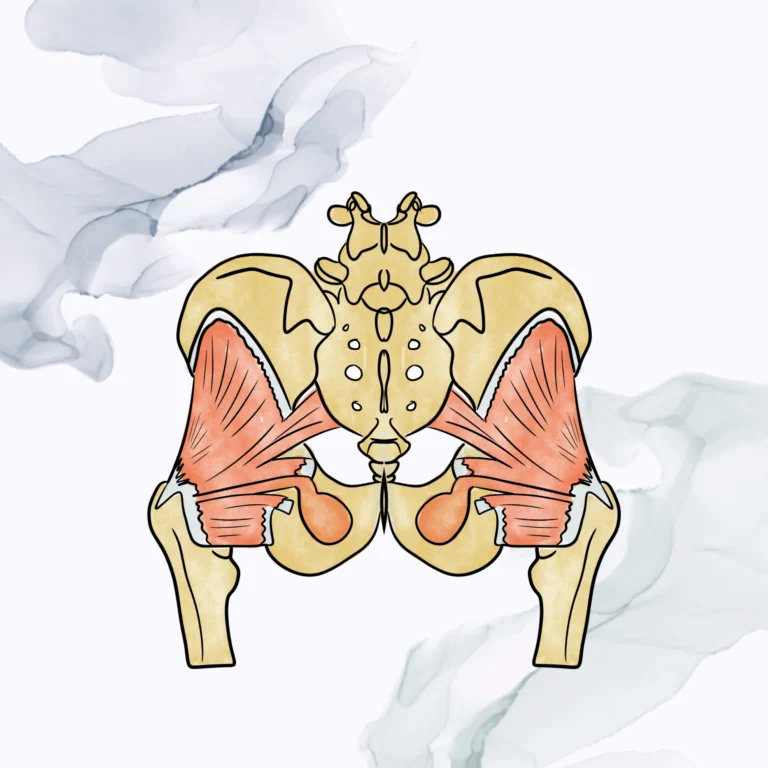
Most types of incontinence (gas, bowel, and bladder) can be helped with pelvic floor physical therapy. Not only does pelvic floor PT address the muscular reasons that incontinence occurs, we also address nerve contributions, connective tissue support, coordination ability, and so much more.
Your symptoms may be similar to friends or family members, but the way we treat patients is completely individualized to assess what will work best for you. Pelvic floor PT can make a significant difference in your incontinence and set a plan in place to manage this through your life span.