Pelvic pain is more than just a physical discomfort—it’s an invisible barrier that can disrupt your daily life, relationships, and career. Whether it’s a dull ache, sharp twinge, or persistent pressure, the effects of pelvic pain can ripple through every aspect of your life, leaving you feeling isolated and frustrated. But you don’t have to endure this pain alone. Understanding its causes and exploring effective treatments can help you reclaim your quality of life.
What Is Pelvic Pain?
Pelvic pain refers to discomfort in the lower abdomen and pelvic region. It can vary from occasional mild discomfort to chronic, debilitating pain that lasts six months or longer. Depending on the cause, pelvic pain can present as:
- Localized Pain: Sharp or stabbing sensations in a specific area.
- Diffuse Pain: A widespread ache or heaviness across the pelvic region.
- Pain with Activity: Discomfort during sitting, standing, walking, or physical activities.
- Associated Symptoms: Pain accompanied by bloating, digestive issues, or urinary urgency.
How Pelvic Pain Impacts Your Life
Living with pelvic pain can take a significant toll on your physical, emotional, and social well-being. Many people find themselves avoiding social gatherings, canceling plans, or missing work due to flare-ups or discomfort. The unpredictable nature of pelvic pain often leads to:
- Reduced Mobility: Simple activities like sitting through a meeting or walking to a social event can become unbearable.
- Social Withdrawal: Fear of pain or embarrassment may cause you to decline invitations or skip outings.
- Workplace Challenges: Concentrating on tasks, attending long meetings, or meeting deadlines becomes increasingly difficult.
- Emotional Strain: Chronic pain can lead to anxiety, depression, or feelings of isolation.
What Causes Pelvic Pain?
Pelvic pain is a complex condition with many potential underlying causes. Identifying the root issue is key to effective treatment. Common contributors include:
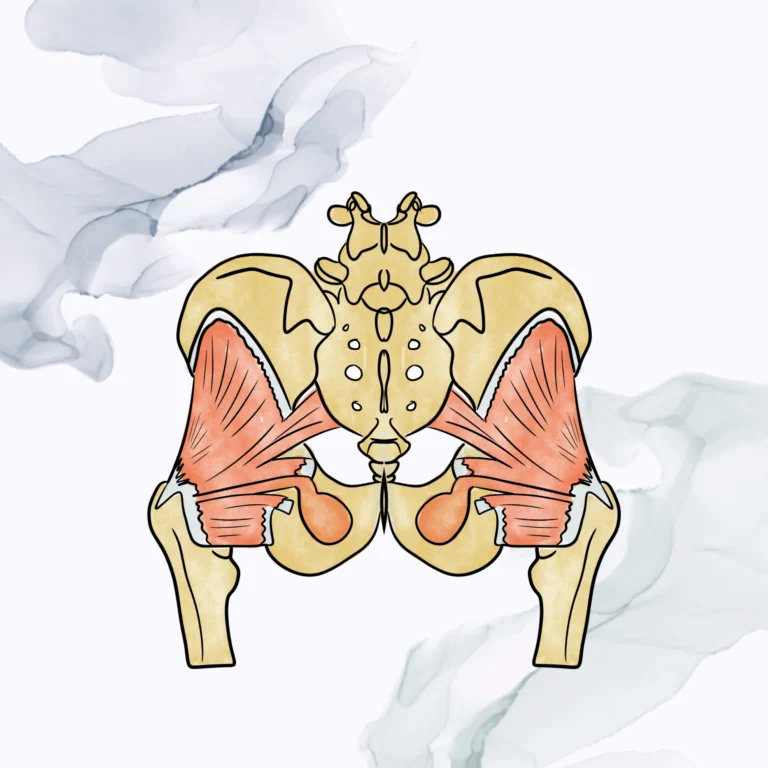
- Pelvic Floor Dysfunction: When the pelvic muscles become overly tight or weak, they can cause pain, pressure, and dysfunction.
- Reproductive System Disorders: Conditions such as endometriosis, ovarian cysts, or pelvic inflammatory disease can lead to chronic discomfort.
- Gastrointestinal Issues: Constipation, irritable bowel syndrome (IBS), or inflammatory bowel disease (IBD) may trigger pelvic pain.
- Urological Conditions: Interstitial cystitis, urinary tract infections (UTIs), or bladder disorders can cause pain and urgency.
- Neurological Causes: Nerve-related pain, such as pudendal neuralgia, often manifests as burning or stabbing sensations.
Why Pelvic Pain Shouldn’t Be Ignored
While it may be tempting to push through the pain or hope it resolves on its own, untreated pelvic pain often worsens over time. Ignoring symptoms can lead to:
- Chronic Pain Cycles: Prolonged pain sensitizes the nervous system, making symptoms harder to treat.
- Increased Emotional Distress: Persistent discomfort often heightens feelings of anxiety, frustration, or hopelessness.
- Reduced Quality of Life: Delaying treatment can result in greater disruptions to your personal, social, and professional life.
Seeking help early is critical for breaking the cycle of pain and restoring your quality of life.
How Pelvic Floor Physical Therapy Can Help
Pelvic floor physical therapy (PFPT) is a highly effective, non-invasive approach to managing and alleviating pelvic pain. By focusing on the muscles, nerves, and tissues of the pelvic region, PFPT addresses both the symptoms and underlying causes of discomfort. A typical treatment plan may include:
- Manual Therapy: Hands-on techniques to release tight muscles, improve blood flow, and reduce trigger points.
- Exercise Programs: Targeted exercises to strengthen weak muscles and improve pelvic alignment.
- Biofeedback: A tool to help you gain awareness and control over pelvic muscle function.
- Education and Support: Learning about the anatomy and triggers of pelvic pain to empower you in your recovery.
When to Seek Help
If pelvic pain is interfering with your ability to work, socialize, or enjoy daily activities, it’s time to seek professional support. Signs that you should consider treatment include:
- Persistent or worsening pain that lasts more than a few weeks.
- Difficulty sitting, standing, or engaging in activities for extended periods.
- Pain that disrupts your sleep or concentration.
- Avoidance of social or professional commitments due to discomfort.
Pelvic pain doesn’t have to dictate your life. With the right support and treatment plan, relief is possible. Addressing the physical and emotional aspects of pain can help you return to the activities and relationships that matter most.