Involuntary urinary or bowel leakage, often referred to as incontinence, is more common than most people realize. Despite its prevalence, it’s a topic many shy away from discussing — but incontinence is manageable and you don’t have to navigate it alone. Understanding the causes and exploring effective treatments can help you reclaim confidence and control.
What Is Incontinence?
Incontinence refers to the loss of control over bladder or bowel functions. It can manifest in different ways, from occasional leakage during physical activity to a persistent inability to manage these bodily functions. This variability means that no two experiences are exactly alike, but they all share a common thread—disruption to daily life.
- Stress Incontinence: Leakage during activities that increase abdominal pressure, such as sneezing, coughing, or exercising.
- Urge Incontinence: A sudden, strong urge to urinate, often followed by leakage.
- Overflow Incontinence: Occurs when the bladder doesn’t empty fully, leading to dribbling.
- Functional Incontinence: Caused by physical or cognitive impairments that make it difficult to reach the restroom in time.
- Fecal Incontinence: The inability to control bowel movements, which may involve occasional or complete loss of control.
Who Experiences Incontinence?
Incontinence can affect anyone, regardless of age or gender. Although it becomes more common with age, it is not an inevitable part of getting older. The condition often arises from underlying factors such as childbirth, surgery, chronic illnesses, or even lifestyle habits.
- Women: Incontinence in women can occur at any stage of life—not just during pregnancy, postpartum, or menopause. Pelvic floor changes, hormonal fluctuations, high-impact exercise, and other stressors can all contribute to leaks.
- Men: Prostate issues or surgeries can contribute to urinary or fecal incontinence.
- Older Adults: Muscle weakening and age-related changes in bladder function are common contributors.
- Active Individuals: High-impact sports such as running, gymnastics, or tennis can place strain on the pelvic floor, increasing the risk of bladder and bowel leakage.
- Chronic Illness Sufferers: Conditions like diabetes, multiple sclerosis, or Parkinson’s disease often impact bladder and bowel control.
Common Causes of Incontinence
Incontinence arises from a combination of physical, medical, and lifestyle factors. Understanding these contributors is essential for finding the right treatment:
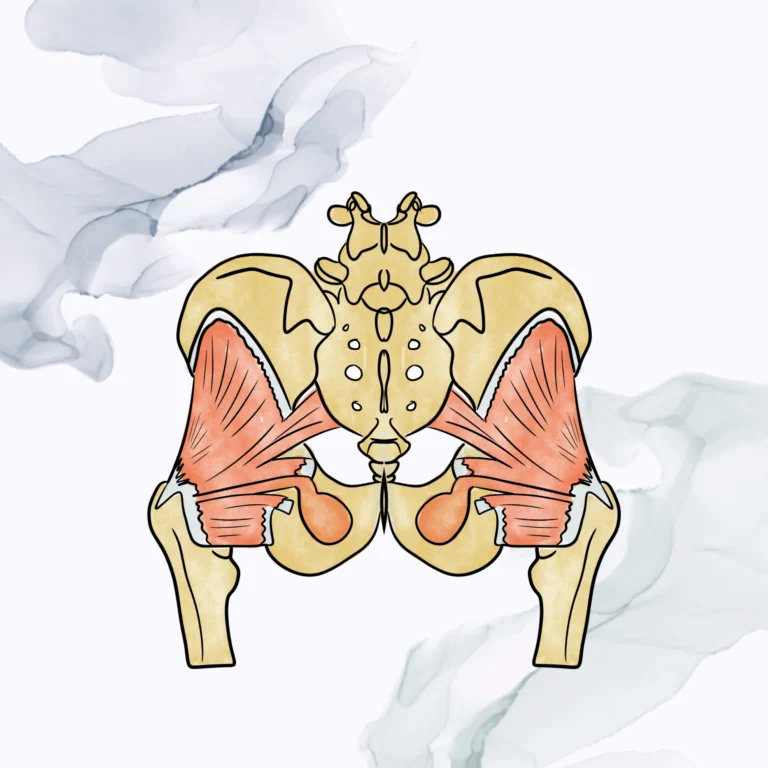
- Pelvic Floor Dysfunction: Weak or overly tense pelvic muscles can disrupt bladder and bowel control.
- Nerve Damage: Caused by surgeries, injuries, or conditions like diabetes, nerve damage can interfere with the signals that regulate urination and defecation.
- Hormonal Changes: Particularly in women, hormonal shifts during menopause can weaken muscle tone.
- Diet and Lifestyle Factors: Excessive caffeine, alcohol, or certain medications may irritate the bladder.
- Underlying Medical Issues: Conditions like urinary tract infections, constipation, or pelvic organ prolapse can exacerbate incontinence.
The Role of Pelvic Floor Physical Therapy
For many, pelvic floor physical therapy (PFPT) is a game-changer. PFPT is a non-invasive, evidence-based approach that focuses on strengthening and retraining the muscles that control bladder and bowel functions. Common treatment paths include:
- Manual Therapy: Hands-on techniques to release muscle tension and improve mobility.
- Biofeedback Training: A tool to help patients identify and control the correct muscles.
- Tailored Exercises: To strengthen weakened pelvic muscles or relax overly tense ones.
- Lifestyle Education: Guidance on habits, posture, and strategies to support pelvic health.
When Should You Seek Help?
It’s essential to recognize when incontinence is more than just an occasional annoyance. If leaks are interfering with your work, social activities, or overall quality of life, it’s time to seek professional guidance. Specific signs to watch for include:
- Frequent urinary or bowel leakage that disrupts daily life.
- Persistent pressure or discomfort in the pelvic area.
- Difficulty completely emptying the bladder or bowel.
- Avoidance of activities due to fear of leaks.
Early intervention is key. Addressing the issue promptly can prevent worsening symptoms and improve outcomes.
Other Treatment Options to Consider
While PFPT is a highly effective starting point, other treatments may complement or enhance your recovery plan depending on the severity of your symptoms:
- Medications: To manage overactive bladder symptoms or treat underlying conditions.
- Medical Devices: Devices like pessaries can provide additional pelvic support.
- Surgical Options: Procedures such as sling surgery or nerve stimulation may be necessary for severe cases.
Living with incontinence can feel like a loss of control, but it doesn’t have to define your life. With advancements in treatments and a growing understanding of pelvic health, relief is more achievable than ever.
At Pelvic Health Solutions, we believe in empowering individuals with the knowledge and support needed to address incontinence effectively. Our team offers compassionate, personalized care designed to meet your unique needs. If you’re ready to take the first step toward reclaiming your freedom and confidence, contact us today.